Garner (919) 661-4150
August 2021
Ingrown Toenails
An ingrown toenail is a nail that has curved downward and grown into the skin. This typically occurs at either the nail borders or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. In most cases, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Is My Ingrown Toenail Infected?
 Ingrown toenails occur when a toenail grows into the surrounding skin instead of over it. While many cases of ingrown toenails can be resolved without complications, it is important to stay on the lookout for any signs of infection. These may include reddening or hardening of the skin surrounding the ingrown nail, swelling, pain, pressure under the nail, throbbing, bleeding, a foul odor, a buildup of fluid, and warmth around the nail. In more severe infections, pus-filled abscesses can form where the nail pokes into the skin. If your ingrown toenail is showing signs of infection, it is suggested that you see a podiatrist as soon as possible.
Ingrown toenails occur when a toenail grows into the surrounding skin instead of over it. While many cases of ingrown toenails can be resolved without complications, it is important to stay on the lookout for any signs of infection. These may include reddening or hardening of the skin surrounding the ingrown nail, swelling, pain, pressure under the nail, throbbing, bleeding, a foul odor, a buildup of fluid, and warmth around the nail. In more severe infections, pus-filled abscesses can form where the nail pokes into the skin. If your ingrown toenail is showing signs of infection, it is suggested that you see a podiatrist as soon as possible.
Ingrown toenails may initially present themselves as a minor discomfort, but they may progress into an infection in the skin without proper treatment. For more information about ingrown toenails, contact Chukwuma Ukata, DPM of Advanced Carolina Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails are caused when the corner or side of a toenail grows into the soft flesh surrounding it. They often result in redness, swelling, pain, and in some cases, infection. This condition typically affects the big toe and may recur if it is not treated properly.
Causes
- Improper toenail trimming
- Genetics
- Improper shoe fitting
- Injury from pedicures or nail picking
- Abnormal gait
- Poor hygiene
You are more likely to develop an ingrown toenail if you are obese, have diabetes, arthritis, or have any fungal infection in your nails. Additionally, people who have foot or toe deformities are at a higher risk of developing an ingrown toenail.
Symptoms
Some symptoms of ingrown toenails are redness, swelling, and pain. In rare cases, there may be a yellowish drainage coming from the nail.
Treatment
Ignoring an ingrown toenail can have serious complications. Infections of the nail border can progress to a deeper soft-tissue infection, which can then turn into a bone infection. You should always speak with your podiatrist if you suspect you have an ingrown toenail, especially if you have diabetes or poor circulation.
If you have any questions, please feel free to contact our office located in Garner, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Do Your Child's Feet Hurt?
How to Care for Your Arthritic Foot
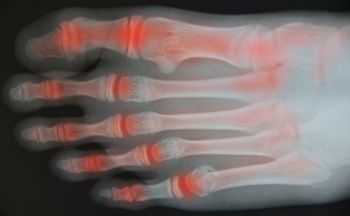
Arthritis is an inflammation of the joints and it can occur at any joint in the body, especially in the foot. It generally effects those who are older, however, it can occur at any age. Although there are many different forms of arthritis, there are three main types that occur in the foot. The three types are osteoarthritis, rheumatoid arthritis, and gout.
The primary cause of osteoarthritis is aging. As you age, cartilage degenerates around the joints which causes friction and pain. Obesity can cause osteoarthritis through mechanical stress. Injuries that damage joints can increase the probability as well. Finally, a family history of osteoarthritis can also increase chances of having it.
Rheumatoid arthritis occurs when the immune system attacks the joint linings and weakens them over a long time. While there is no known cause of rheumatoid arthritis, obesity and smoking can increase your chances of getting it. Women are also more likely to get it than men.
Gout is a form of arthritis that occurs when there is too much uric acid in your blood and painful crystals form in your joints. Men are more likely to have gout than women. People who are obese or drink alcohol often are also more likely to develop gout. Furthermore, having diabetes, heart disease, high blood pressure, high cholesterol, gastric bypass surgery or a family history of gout may increase your likelihood of developing the condition.
Symptoms of arthritis include pain, stiffness, swelling in the joints. These symptoms can make it harder and more painful to walk. Physical activity can increase pain and discomfort. Furthermore, joint pain can worsen throughout the day for osteoarthritis. Gout attacks generally last several days with the first few being the worst.
Diagnosis of gout includes either a joint fluid test or a blood test. X-ray imaging can detect osteoarthritis but not gout. On the other hand, there is no blood test for osteoarthritis. Rheumatoid arthritis is difficult to diagnosis. Doctors utilize family and personal medical history, a physical examination, and antibody blood tests to determine if you have rheumatoid arthritis.
Treatment varies for the different kinds of arthritis. Anti-inflammatory medication or steroids can help reduce pain from inflammation of the joints. Changing shoe types can help with some symptoms. Wider shoes can help with discomfort from gout and osteoarthritis. High heels should be avoided. Shoes with proper arch support and that take pressure off the ball of the foot can help with rheumatoid arthritis. Drinking lots of water can also help rid uric acid from the blood. Losing weight, improving your diet, and limiting alcohol and smoking can also help prevent or lessen the symptoms of arthritis.
If you are having trouble walking or pain in your feet, see a podiatrist to check if you have arthritis.
Walking May Help With Symptoms of Arthritis
 Research has suggested that walking may be one of the best methods to manage the symptoms of pain, stiffness, or inflammation that can coincide with arthritis. It is important to start off slowly by building a walking routine, and with some time and experience, it should become easier when performed every day. Walking can also be beneficial for losing weight which may help lessen the stress that the joints endure. Slowly increasing the frequency, intensity, and length of time that you walk is the preferred method and can help to alleviate the aches and pain from arthritis. Many patients find that counting how many steps they take every day can help track their daily progress for maximum benefits. If you have arthritis in your feet, it is strongly suggested that you consult with a podiatrist who can offer you proper management techniques.
Research has suggested that walking may be one of the best methods to manage the symptoms of pain, stiffness, or inflammation that can coincide with arthritis. It is important to start off slowly by building a walking routine, and with some time and experience, it should become easier when performed every day. Walking can also be beneficial for losing weight which may help lessen the stress that the joints endure. Slowly increasing the frequency, intensity, and length of time that you walk is the preferred method and can help to alleviate the aches and pain from arthritis. Many patients find that counting how many steps they take every day can help track their daily progress for maximum benefits. If you have arthritis in your feet, it is strongly suggested that you consult with a podiatrist who can offer you proper management techniques.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Chukwuma Ukata, DPM from Advanced Carolina Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our office located in Garner, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Bunions
A bunion is a bump that forms at the base of the big toe. Bunions form when the big toe pushes against the next toe, which forces the big toe joint to get bigger and stick out. As a result, the skin over the bunion may start to appear red and it may feel sore.
There are risk factors that can increase your chances of developing bunions. People who wear high heels or ill-fitting shoes are more likely to develop them, in addition to those who have a genetic history of bunions or have rheumatoid arthritis.
The most obvious way to tell if you have a bunion is to look for the big toe pushing up against the toe next to it. Bunions produce a large protrusion at the base of the big toe and may or may not cause pain. Other symptoms are redness, swelling, and restricted movement of the big toe if you have arthritis.
Nonsurgical methods are frequently used to treat bunions that aren’t severe. Some methods of nonsurgical treatment are orthotics, icing and resting the foot, taping the foot, and pain medication. Surgery is usually only required in extreme cases. However, if surgery is needed, some procedures may involve removing the swollen tissue from around the big toe joint, straightening the big toe by removing part of the bone, or joining the bones of your affected joint permanently.
Your podiatrist will diagnose your bunion by doing a thorough examination of your foot. He or she may also conduct an x-ray to determine the cause of the bunion and its severity.
Are You Experiencing Bunion Pain?
 A bunion is a bony bump that can form at the base of the big toe joint. Many people believe that bunions are a strictly cosmetic issue, only affecting the way that the foot looks, but bunions can also be painful and lead to other foot problems that may interfere with your day-to-day life. A bunion can push your big toe towards the smaller ones, changing the shape of the foot and making the big toe joint sore, stiff, swollen, or inflamed. Blisters, corns, and calluses may form in between or on top of the toes as your shoe rubs against the bunion. All of these symptoms can lead to difficulty walking and going about your daily activities. Furthermore, bunions can increase your risk of other potentially painful foot problems, including hammertoes, bursitis, and metatarsalgia. Bunions tend to worsen over time, so if you notice a bunion forming on your foot, it is suggested that you see a podiatrist for treatment as soon as possible.
A bunion is a bony bump that can form at the base of the big toe joint. Many people believe that bunions are a strictly cosmetic issue, only affecting the way that the foot looks, but bunions can also be painful and lead to other foot problems that may interfere with your day-to-day life. A bunion can push your big toe towards the smaller ones, changing the shape of the foot and making the big toe joint sore, stiff, swollen, or inflamed. Blisters, corns, and calluses may form in between or on top of the toes as your shoe rubs against the bunion. All of these symptoms can lead to difficulty walking and going about your daily activities. Furthermore, bunions can increase your risk of other potentially painful foot problems, including hammertoes, bursitis, and metatarsalgia. Bunions tend to worsen over time, so if you notice a bunion forming on your foot, it is suggested that you see a podiatrist for treatment as soon as possible.
If you are suffering from bunion pain, contact Chukwuma Ukata, DPM of Advanced Carolina Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our office located in Garner, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
Stress Fractures in the Front of the Foot
There are five long metatarsal bones in the front of the foot which connect the toes with the tarsal bones of the mid-and-hind-foot. These metatarsals bear a great deal of weight during walking, running and jumping, which makes them more susceptible to tiny cracks known as stress fractures. These stress fractures occur over time through repetitive activity which first weakens, and eventually cracks these metatarsals. Stress fractures in the metatarsals can be caused by osteoporosis or other activities that can weaken bones, irregular body mechanics (how the body moves), or a sudden change in physical activity. Symptoms of a stress fracture can include discomfort ranging from a dull ache to a sharp pain which may wax and wane, along with bruising or swelling. If you are experiencing pain in the front of your foot, or any part of your foot, a podiatrist can help diagnose and treat your condition.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact Chukwuma Ukata, DPM from Advanced Carolina Foot and Ankle Center. Our doctor can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our office located in Garner, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ankle Foot Orthotics for Athletes
Ankle foot orthotics are shoe inserts that offer support to control the placement and movement of the ankle, correct deformities, and compensate for weakness. These inserts are used to stabilize the foot and ankle and provide toe clearance during the swing phase of gate.
Athletes often suffer foot problems because their feet are not being supported within the shoe. Ankle and foot orthotics are custom made inserts that alleviate stress on the foot. However custom orthotics should be prescribed by a podiatrist who specializes in customized footwear and orthotics design. These inserts are used by athletes for different reasons. Runners use orthotics to absorb shock at heel contact and to set up the forefoot for push-off. Basketball players wear them to control their forefeet while jumping and running.
The two main types of orthotics are over-the-counter orthotics and custom-made orthotics. To be eligible for custom orthotics, an examination of the foot and ankle will need to be completed. Afterward, both the foot and ankle will need to be casted and fitted for the proper orthotic. When the fitting process is complete, adjustments can be made to make sure everything fits perfectly.
Over the counter orthotics tend to be more popular than custom fit ones. Athletes who have less severe aches and pains in the foot, ankle or lower back area can use the over-the-counter version of orthotics. Unfortunately, over-the-counter orthotics tend to not work in treating severe injuries or ailments. Whenever you suspect you may need an ankle foot orthotic, you should consult with your podiatrist to determine which type of orthotic is right for you.