Garner (919) 661-4150
An Overview of Heel Spurs
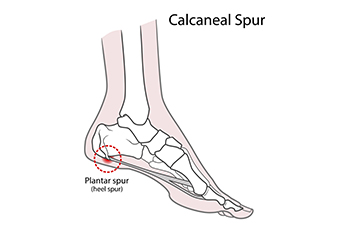
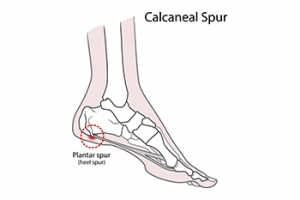
A heel spur is a common foot condition that is often discussed in the context of heel pain and discomfort. Despite their reputation, they are not actually sharp, pointy growths, as the term may imply. Instead, heel spurs are calcium deposits that form on the underside of the heel bone. These deposits often develop over an extended period of time due to chronic inflammation or stress on the plantar fascia, the band of tissue that connects the heel to the toes. The primary characteristic of heel spurs is the accompanying pain. This discomfort is often described as a sharp, stabbing sensation, particularly with the first steps in the morning or after prolonged periods of rest. It is important to note that not everyone with heel spurs experiences pain, as many people have them without any symptoms. The causes of heel spurs are diverse, with factors such as obesity, gait abnormalities, or wearing inadequate footwear contributing significantly. Heel spurs are a condition that is often linked to heel pain, but they are generally not the sole cause. If you are experiencing persistent heel pain, it is suggested that you consult a podiatrist, who can accurately diagnose and treat heel spurs if they are the culprit.
Heel spurs can be incredibly painful and sometimes may make you unable to participate in physical activities. To get medical care for your heel spurs, contact Chukwuma Ukata, DPM from Advanced Carolina Foot and Ankle Center. Our doctor will do everything possible to treat your condition.
Heels Spurs
Heel spurs are formed by calcium deposits on the back of the foot where the heel is. This can also be caused by small fragments of bone breaking off one section of the foot, attaching onto the back of the foot. Heel spurs can also be bone growth on the back of the foot and may grow in the direction of the arch of the foot.
Older individuals usually suffer from heel spurs and pain sometimes intensifies with age. One of the main condition's spurs are related to is plantar fasciitis.
Pain
The pain associated with spurs is often because of weight placed on the feet. When someone is walking, their entire weight is concentrated on the feet. Bone spurs then have the tendency to affect other bones and tissues around the foot. As the pain continues, the feet will become tender and sensitive over time.
Treatments
There are many ways to treat heel spurs. If one is suffering from heel spurs in conjunction with pain, there are several methods for healing. Medication, surgery, and herbal care are some options.
If you have any questions feel free to contact our office located in Garner, NC . We offer the latest in diagnostic and treatment technology to meet your needs.
Is Your Heel Pain From Plantar Fasciitis?

Determining the root cause of heel pain can be challenging, especially when other conditions like arthritis or tarsal tunnel syndrome come into play. Plantar fasciitis is a leading culprit behind heel pain. It is characterized by sharp pain, inflammation, and tenderness in the sole of the foot, particularly near the heel. Notably, the pain is most pronounced during the first few steps in the morning or after prolonged periods of sitting. Unlike osteoarthritis, which tends to worsen with movement, plantar fasciitis pain often improves as you walk around but worsens later in the day. The condition arises when the plantar fascia, the ligament connecting the heel to the ball of the foot, loses its elasticity and develops tiny tears. These tears lead to painful swelling in the ligament. Diagnosis by a podiatrist may involve a thorough medical history, a physical examination, including range-of-motion tests, and sometimes an X-ray. The good news is that most people with plantar fasciitis find relief through non-invasive, non-surgical treatments. If you suspect you may have developed plantar fasciitis, it is suggested that you make an appointment with a podiatrist for an exam, a diagnosis, and suggested treatment options.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Chukwuma Ukata, DPM from Advanced Carolina Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Garner, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes of Running Injuries

Running is thought to be a good way to stay fit and healthy, but it also comes with risks. Foot and ankle injuries are all too common among runners. Overuse is a prevalent issue, usually stemming from pushing your body too hard or increasing your mileage too quickly. These actions can lead to problems like plantar fasciitis, Achilles tendonitis, and stress fractures. Poor footwear choices also play a significant role in causing foot or ankle injuries. Worn-out or ill-fitting shoes fail to provide the necessary support and cushioning, increasing the risk of injuries. Ensuring your shoes are the right fit for your feet and running style is important. Inadequate warm-up routines can strain the muscles and ligaments, making them more susceptible to injuries. In addition, running on uneven terrain can increase the likelihood of twisting an ankle. Biomechanical issues, such as overpronation or supination, can place extra stress on your feet and ankles, making them prone to injury. If you experience persistent pain or discomfort as a result of your running activity, it is suggested that you consult a podiatrist for an exam, diagnosis, and treatment options.
Exercising your feet regularly with the proper foot wear is a great way to prevent injuries. If you have any concerns about your feet, contact Chukwuma Ukata, DPM of Advanced Carolina Foot and Ankle Center. Our doctor will treat your foot and ankle needs.
How to Prevent Running Injuries
Many common running injuries are caused by overuse and overtraining. When the back of the kneecap starts wearing out and starts causing pain in your knee, this is commonly referred to as runner’s knee. Runner’s knee is a decrease in strength in your quadriceps and can occur if you’re not wearing properly fitted or supporting shoes. To prevent runner’s knee, focusing on hip strengthening is a good idea, as well as strengthening your quads to keep the kneecaps aligned.
What Are Some Causes of Running Injuries?
- One cause of a common running injury is called iliotibial band syndrome.
- Plantar fasciitis is also another common injury.
- Stress fractures can occur from overtraining, lack of calcium, or even your running style.
Best Ways to Prevent Running Injuries
- Wear footwear that fits properly and suits your running needs.
- Running shoes are the only protective gear that runners have to safeguard them from injury.
- Make a training schedule. Adding strengthening exercises as well as regular stretching can help keep you strong and limber and can lessen the possibility of injuries.
- Stretching keeps muscles limber; this will help you gain better flexibility.
If you have any questions please feel free to contact our office located in Garner, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How Rheumatoid Arthritis Affects the Feet

Rheumatoid arthritis, abbreviated RA, is a relentless autoimmune disorder that does not spare the feet from pain. The immune system's misguided attacks on the synovium, which is the protective lining of joints, lead to chronic inflammation in various parts of the body, including the feet. The small joints in the toes, the arch, and the ankle are frequent targets, causing swelling, stiffness, and pain. Over time, RA can lead to deformities, such as bunions, hammertoes, and collapsed arches, resulting in altered foot structure and gait. The chronic pain can impair mobility, leading to a reduced quality of life. Early diagnosis and prompt intervention are crucial to managing symptoms and slowing down the progression. A treatment approach involving medication, wearing orthotics, and incorporating lifestyle adjustments may help to alleviate the burden on the feet and enhance overall foot health for individuals with RA. If you have this condition, it is strongly suggested that you are under the care of a podiatrist who can offer you additional relief options.
Because RA affects more than just your joints, including the joints in your feet and ankles, it is important to seek early diagnosis from your podiatrist if you feel like the pain in your feet might be caused by RA. For more information, contact Chukwuma Ukata, DPM of Advanced Carolina Foot and Ankle Center. Our doctor will assist you with all of your podiatric concerns.
What Is Rheumatoid Arthritis?
Rheumatoid Arthritis (RA) is an autoimmune disorder in which the body’s own immune system attacks the membranes surrounding the joints. Inflammation of the lining and eventually the destruction of the joint’s cartilage and bone occur, causing severe pain and immobility.
Rheumatoid Arthritis of the Feet
Although RA usually attacks multiple bones and joints throughout the entire body, almost 90 percent of cases result in pain in the foot or ankle area.
Symptoms
- Swelling and pain in the feet
- Stiffness in the feet
- Pain on the ball or sole of feet
- Joint shift and deformation
Diagnosis
Quick diagnosis of RA in the feet is important so that the podiatrist can treat the area effectively. Your doctor will ask you about your medical history, occupation, and lifestyle to determine the origin of the condition. Rheumatoid Factor tests help to determine if someone is affected by the disease.
If you have any questions please feel free to contact our office located in Garner, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Rheumatoid Arthritis in the Feet
Rheumatoid Arthritis is a chronic progressive disease that attacks several joints throughout the body. It is an autoimmune disease in which the body’s immune system mistakenly attacks the joints. As a result, the tissue inside the joints, called synovium, starts to thicken and causes pain around the joints. The synovium is responsible for creating a fluid that lubricates the joints to help them move. Approximately 1.5 million people in the United States have Rheumatoid Arthritis. Women are almost three times as likely to have RA compared to men, and it’s disease usually begins between the ages of 30 and 60. People who have a genetic history of RA are more likely to develop the disease.
Symptoms of RA may include the following sensations in the joints: pain, tenderness, swelling, redness, warmth, stiffness, and loss of range. Swollen joints are a very common symptom for those with the disease. At times, it may be minimal, but it may also be very apparent. Another typical symptom is joint stiffness. Doctors will often use the direction of morning stiffness to measure the severity of a patient’s joint inflammation. Other RA symptoms include limping, anemia, fever, and fatigue.
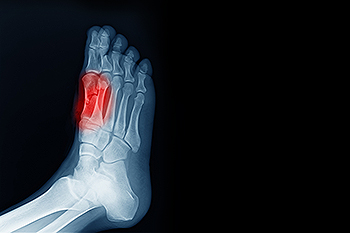
To diagnose RA, your podiatrist will typically request x-rays to see how much damage there is in the joints. Blood tests may also be performed to show if there are any signs of anemia, or antibodies such as the rheumatoid factor. If you have previously been diagnosed with RA, you should know the disease may spread to your feet and ankles.
There are many non-surgical options that can be used to treat this ailment. Some of these options include physical therapy, foot massages, orthotics, bracing, supportive shoes, and steroid injections. Physical therapy is useful because it will help stretch and strengthen the joints in both the foot and ankle to improve joint function. Massages can help improve blood circulation which will be good for the feet. Choosing proper footwear will allow you to walk with comfortability if you are a sufferer from RA. Lastly, bracing will help stabilize the foot joints, limit deformities and decrease pain.
In severe cases, surgery may be a treatment option that should be considered. For those who cannot walk without experiencing pain and those whose deformities can not be managed with braces, surgery should be considered. Your podiatrist will recommend surgery if he or she believes it will improve your foot biomechanics.
Finding the Right Running Shoes for Sesamoiditis
Many athletes, such as runners, and dancers, experience a condition known as sesamoiditis. This is an inflammation of the tendons of two tiny sesamoid bones that lie under the big toe joint. Any activity that transfers weight to the ball of the foot can cause sesamoiditis. Runners with this condition may need help in finding the proper shoes to accommodate this overuse injury. Such a shoe would likely have a wide toe box that allows the toes to spread wider than the ball of the foot. Secondly, it would include what is termed by experts as a zero heel-to-toe drop. In effect, the ball of the foot and heel would be aligned on the same plane. Lastly, the shoe should not have an elevation of the toe box above the ground, which is termed a toe spring. The current industry toe spring standard is 15 degrees. This can increase pressure on the ball of the foot. While it may be difficult to adjust to this type of minimalist running shoe, some people may wish to ease into the change with transition shoes. If you have any questions on how to deal with sesamoiditis and find the shoe that can keep you running, it is suggested that you make an appointment with a podiatrist.
Sesamoiditis is an unpleasant foot condition characterized by pain in the balls of the feet. If you think you’re struggling with sesamoiditis, contact Chukwuma Ukata, DPM of Advanced Carolina Foot and Ankle Center. Our doctor will treat your condition thoroughly and effectively.
Sesamoiditis
Sesamoiditis is a condition of the foot that affects the ball of the foot. It is more common in younger people than it is in older people. It can also occur with people who have begun a new exercise program, since their bodies are adjusting to the new physical regimen. Pain may also be caused by the inflammation of tendons surrounding the bones. It is important to seek treatment in its early stages because if you ignore the pain, this condition can lead to more serious problems such as severe irritation and bone fractures.
Causes of Sesamoiditis
- Sudden increase in activity
- Increase in physically strenuous movement without a proper warm up or build up
- Foot structure: those who have smaller, bonier feet or those with a high arch may be more susceptible
Treatment for sesamoiditis is non-invasive and simple. Doctors may recommend a strict rest period where the patient forgoes most physical activity. This will help give the patient time to heal their feet through limited activity. For serious cases, it is best to speak with your doctor to determine a treatment option that will help your specific needs.
If you have any questions please feel free to contact our office located in Garner, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What Is Kohler Disease?

Kohler disease is categorized as a rare foot condition. It is considered to be a bone disorder and can result from compression caused by stress during a critical growth period. A common symptom of this condition is a swollen foot, which can be painful. It may be especially sensitive in the arch of the foot, which can appear to be red. Children between the ages of 3 and 7 are generally affected by Kohler disease, and parents may notice their child is limping. Walking can be difficult, and this may be from an interruption of blood flow to one of the bones in the foot. Research has shown the exact cause of Kohler disease is not known, but some specialists speculate it can be related to an injury that may have occurred before the child was 2 years old. Many cases of Kohler disease will gradually resolve, and the time frame can depend on the severity of the symptoms. If your child has a swollen foot, it is suggested that you consult with a podiatrist who can diagnose and treat this rare foot condition.
Some foot conditions may require additional professional care. If you have any concerns, contact Chukwuma Ukata, DPM of Advanced Carolina Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Rare Foot Conditions
The majority of foot conditions are common and can be treated by a podiatrist. Standard diagnostic procedures are generally used to identify specific conditions and treatment can be rendered. A podiatrist also treats rare foot conditions which can be difficult to diagnose and may need extra attention and care.
There are many rare foot conditions that can affect children. Some of these can include:
- Freiberg’s disease
- Kohler’s disease
- Maffucci syndrome
Freiberg’s disease - This can be seen as a deterioration and flattening of a metatarsal bone that exists in the ball of the foot. It typically affects pre-teen and teenage girls, but can affect anyone at any age. Symptoms that can accompany this can be swelling, stiffness, and the patient may limp.
Kohler’s disease - This often targets the bone in the arch of the foot and affects younger boys. It can lead to an interruption of the blood supply which ultimately can lead to bone deterioration. The patient may limp or experience tenderness, swelling, and redness.
Maffucci syndrome - This affects the long bones in a child’s foot leading to the development of abnormal bone lesions. They are benign growths and typically develop in early childhood and the bones may be susceptible to breaking.
A podiatrist can properly diagnose and treat all types of rare foot conditions. If your child is affected by any of these symptoms or conditions, please don’t hesitate to call our office so the correct treatment method can begin.
If you have any questions please feel free to contact our office located in Garner, NC . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Rare Foot Conditions
A podiatrist will be able to address a variety of rare foot conditions, particularly the ones that affect children. The most common are Kohler’s disease, Maffucci syndrome, and Freiberg’s disease. They can be properly diagnosed by having an X-ray taken, but in more serious cases an MRI may be needed. Kohler’s disease generally affects younger boys and bone deterioration may result from an interruption of blood supply. Children who have Kohler’s disease may find relief when the affected foot is rested, and a special boot is worn. Benign growths in the long bones of a child’s foot may lead to the development of bone lesions, and this is known as Maffucci syndrome. People who have this condition find mild relief when custom-made orthotics are worn. Freiberg’s disease targets the ball of the foot and can typically affect pre-teen and teenage girls. The metatarsal bone becomes deteriorated and flattened, and common symptoms include swelling and stiffness. A cast is often necessary to wear with this disease as it can help to reduce existing pain. Erythromelalgia is a rare foot condition, and its cause is unknown. Symptoms of this disease can include intense burning pain and the feet may appear red or feel warm. Relief may be found when the affected foot is immersed in ice water. It can also be beneficial to elevate the foot frequently. If your child complains of foot pain, it is strongly suggested that you consult with a podiatrist who can diagnose and treat rare foot conditions.
Men Are More Prone to Getting Gout

Anyone is at risk for getting the foot condition that is known as gout, despite it being more prevalent among men. The chances may increase in women after menopause, and it generally does not happen before then. Existing medical conditions may lead to developing gout, including obesity, alcoholism, and high blood pressure. A genetic history may also contribute to getting gout, in addition to eating foods that have high levels of purines. These types of foods consist of red meat, shellfish, and drinks that are made with large amounts of sugar. The purines convert to uric acid in the blood, and excess uric acid turns to crystals which can lodge in the joints of the big toe. This can cause debilitating pain, and it may be so severe it can be difficult to walk up steps. If you have had one or more bouts of gout, it is strongly suggested that you are under the care of a podiatrist who can effectively treat this condition.
Gout is a painful condition that can be treated. If you are seeking treatment, contact Chukwuma Ukata, DPM from Advanced Carolina Foot and Ankle Center. Our doctor will treat your foot and ankle needs.
What Is Gout?
Gout is a form of arthritis that is characterized by sudden, severe attacks of pain, redness, and tenderness in the joints. The condition usually affects the joint at the base of the big toe. A gout attack can occur at any random time, such as the middle of the night while you are asleep.
Symptoms
- Intense Joint Pain - Usually around the large joint of your big toe, and it most severe within the first four to twelve hours
- Lingering Discomfort - Joint discomfort may last from a few days to a few weeks
- Inflammation and Redness -Affected joints may become swollen, tender, warm and red
- Limited Range of Motion - May experience a decrease in joint mobility
Risk Factors
- Genetics - If family members have gout, you’re more likely to have it
- Medications - Diuretic medications can raise uric acid levels
- Gender/Age - Gout is more common in men until the age of 60. It is believed that estrogen protects women until that point
- Diet - Eating red meat and shellfish increases your risk
- Alcohol - Having more than two alcoholic drinks per day increases your risk
- Obesity - Obese people are at a higher risk for gout
Prior to visiting your podiatrist to receive treatment for gout, there are a few things you should do beforehand. If you have gout you should write down your symptoms--including when they started and how often you experience them, important medical information you may have, and any questions you may have. Writing down these three things will help your podiatrist in assessing your specific situation so that he or she may provide the best route of treatment for you.
If you have any questions, please feel free to contact our office located in Garner, NC . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Tarsal Tunnel Syndrome

Tarsal tunnel syndrome or TTS is when the posterior tibial nerve in the ankle becomes compressed. This can happen from medical conditions including rheumatoid arthritis and diabetes, repetitive stress activities, other foot conditions, or carrying excessive weight. While there is a higher incidence of this ailment among women and adults, it can happen to anyone. When this happens, pain, tingling, and numbness can radiate to the foot and worsen with walking. Rest is helpful when pain develops. This affliction is relatively uncommon and can be misdiagnosed. Because of this, if you have pain in your ankle or heel, it is strongly suggested that you see a podiatrist who can properly evaluate what is causing it and provide treatment options.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Chukwuma Ukata, DPM of Advanced Carolina Foot and Ankle Center. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our office located in Garner, NC . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.